gartner’s duct cysts
 Gartner's duct cysts: a review of surgical management and a new technique using fluorescein dye | SpringerLink
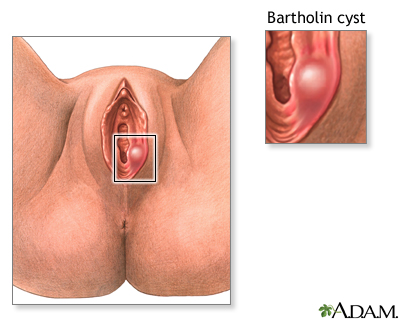
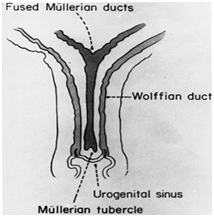
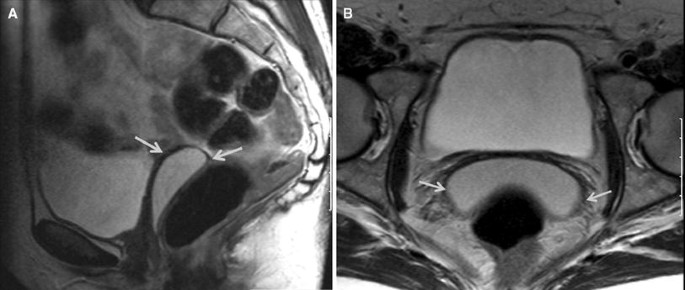
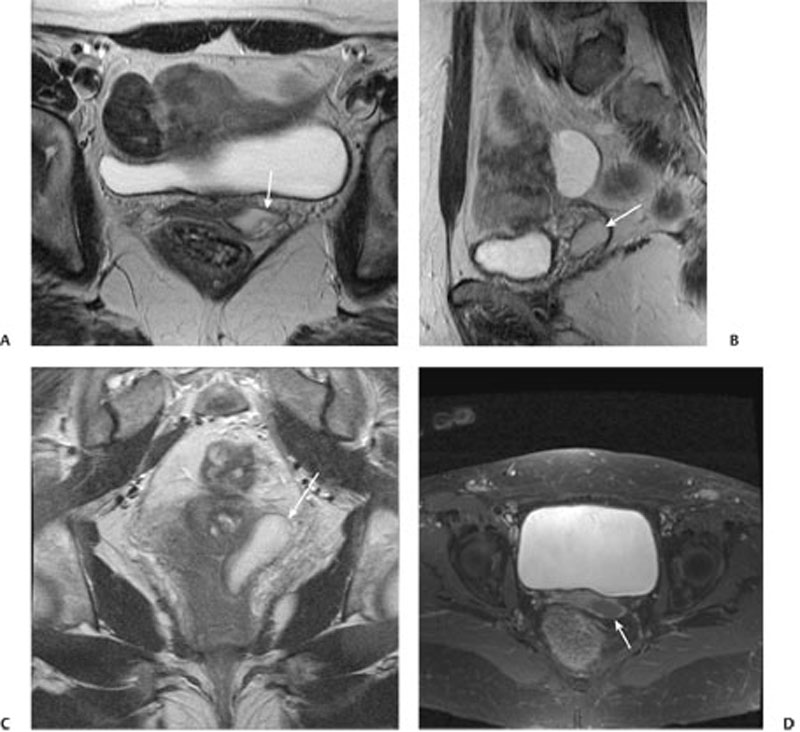
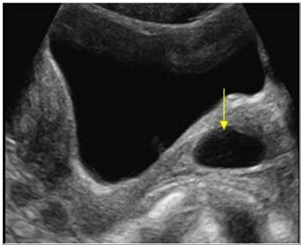
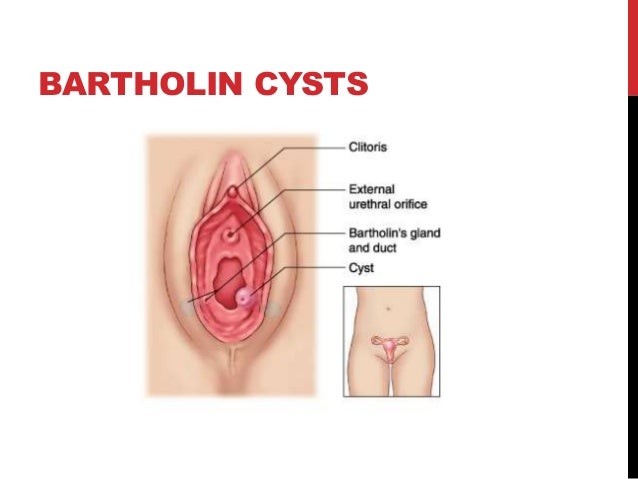
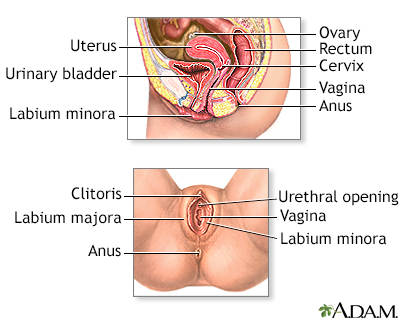
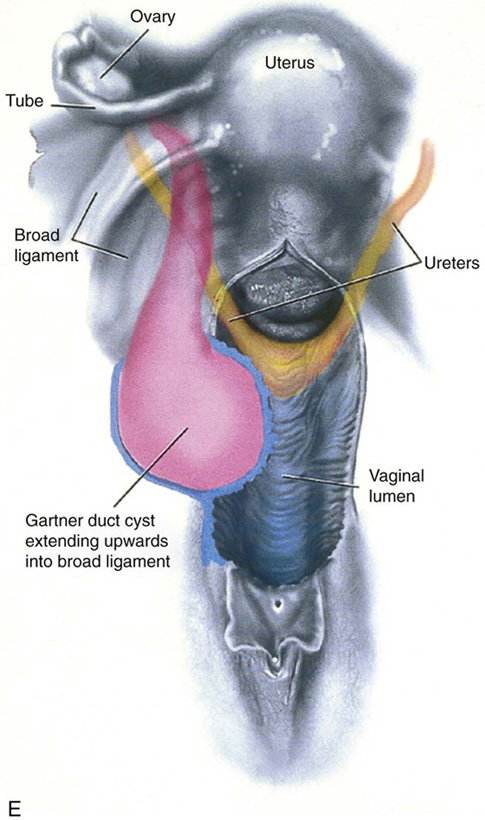
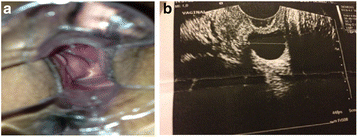
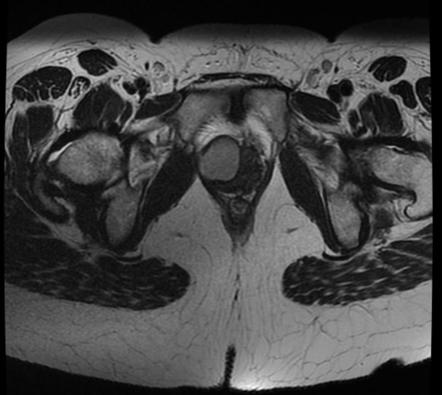
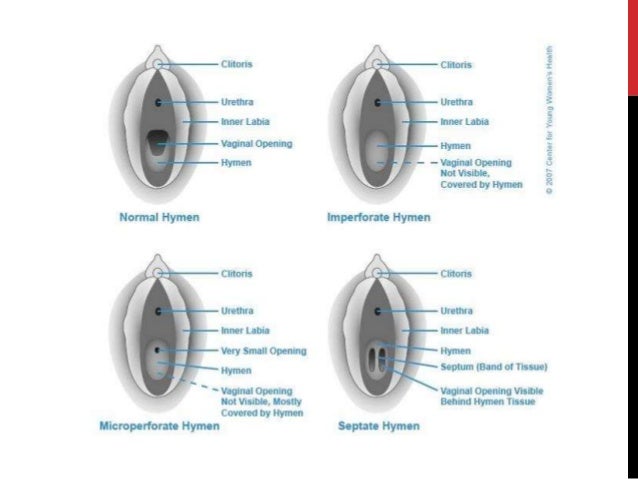
Gartner's duct cysts: a review of surgical management and a new technique using fluorescein dye | SpringerLinkAdvertising Conservative treatment and follow-up of Gartner vaginal duct cysts: a series of cases volume 10, article number: 147 (2016) volume 1028k Accesses3 AltmetricAbstractBackground In women, during embryonic development, Müllerian's peered ducts (paramesonephric) merge distally and develop in the uterus, cervix and upper vagina. If the Wolffian ducts persist in vestigeal form, they can lead to the Gartner cysts, mainly located on the right wall of the vagina. This is one of the few studies of Gartner cysts with a series of consecutive cases for a long period of time that were exclusively subject to clinical observation. Although Gartner's cysts are around 0.1 to 0.2 per cent of women, there is controversy over the course of action to be taken. Case presentation We describe the cases of four women aged 38, 53, 37 and 49 years of age in their first appointment and who were of mixed ethnicity, mixed ethnicity, black ethnicity and mixed ethnicity respectively. The follow-up of these patients varied from 2 to 17 years. In these four cases the location of cysts was the right wall of the vagina. Transvaginal ultrasound was the test of choice for diagnostic confirmation. In the cases presented in this study, women were asymptomatic and decided to be clinically observed. Conclusions This is the first study that reports long-term clinical observation of these lesions. This study shows that conservative treatment can be a safe choice for asymptomatic patients with Gartner vaginal duct cysts. Background The internal urogenital tract is derived from two sets of ducts: Wolffian ducts (mesonephric) and Müllerian ducts (paramesonephric). These ducts are present in both sexes. In women, during the eighth week of embryonic development, the Müllerian ducts paired (paramesonephric) merge distally and develop in the uterus, cervix and upper vagina. In addition, the Wolffian ducts go back. If the ducts persist in a vestigeal form, they can form Gartner cysts. These cysts are mainly found on the right anterolateral wall of the vagina and less commonly on the side walls of the uterus [, ]. The imperfect development of the Wolffian ducts can also result in urogenital anomalies, such as changes in the metanic urinary system [, ]. Cases of ectopian ureter, unilateral renal dysgenesis and renal hypoplasia have also been reported in association with Gartner cysts [, ]. Most of these lesions are asymptomatic, but may be accompanied by infections, bladder dysfunction, abdominal pain, vaginal discharge, and urinary incontinence due to the extrinsic compression of the bladder's neck []. True Gartner duct cysts are typically located along the aterolateral wall of the proximal velvet of the vagina. In contrast, Bartholin cysts are typically found on the lower third posterolateral wall of the vagina and are associated with the larger lips [, ]. The differential diagnosis could include the cyst of the Bartholin gland, uterine prolapse, cytocele, rectum, enterocele, urethral diverticulum, endometriosis and malignant growth, among others []. Although vaginal cysts are found in about 1 to 2 % of women and the Gartner duct cysts comprise about 10 % of the vaginal benign cysts [, ], there is still some controversy about which course of action should be taken. This is the first study to report long-term clinical observation of these injuries. Case presentation Case 1 - 17-year follow-up A 38-year-old mixed-ethnic woman initially referred to our service at 21-year-olds for evaluation before beginning contraceptive use. She reported menarche to the first 13 sexual intercourses at 21 and regular cycles. No abnormalities were observed during a breast exam. A spectra test revealed an epithelialized cervix and the presence of a paracervical cystic lesion on the right wall of your vagina, indolore to manipulation, measuring approximately 2 × 2 cm, with translucent content and soft consistency (Fig. ). An ultrasound revealed a cystic lesion. Regular annual surveillance continued. She became pregnant at the age of 32 and was delivered by caesarean. The cyst remained about 1.5 to 2.0 cm in size and did not change during pregnancy. He's been following up since then, and Gartner's cyst hasn't shown any changes in his features. Fig. 1 Paracervical cystic lesions with translucent content on the right wall of the vagina, of approximately 2 × 2 cmCase 2 – follow-up for 13 yearsA 53-year-old G3P3 woman, mixed ethnicity, sought our service at 40 years of age for a routine visit. He had no significant medical history. After a spectra examination, a cystic lesion was found on the right wall of your vagina with translucent content and extensive vascularization (Fig. ). A transvaginal ultrasound revealed a hypoeco nodule in the vaginal fornix of 4.2 × 3.8 × 2.1 cm, with thick content, and was consistent with a cyst. The removal was advised due to thick content and exuberant vascularization, but she declined. He has been followed to date without alterations. Fig. 2Cystic injury in right wall of the vagina with translucent content, but with exuberant vascularization Case 3 – follow-up for 5 yearsA 37-year-old black woman presented to our service at 32 years for a Pap test. Its obstetric/ginecological history was significant for menarchy at the age of 13, first sexual contact at the age of 15, and regular menstrual cycles. Their pregnancies included a natural delivery, a tubal and an anembrionic pregnancy. He had a left salpingectomy. He also had a history of urethrality that led to recurrent urinary tract infections (UTIs). Her family history points to an aunt with unspecified urethral alterations. Your spectra test revealed a healthy cervix and the presence of a cyst of approximately 2.5 × 2 cm in the proximal third of the right wall of your vagina (Fig. ). The touch revealed a lesion with cystic consistency. He subjected himself to an ultrasound that showed a thin wall cyst with anecoic content on the right side wall of his vagina (Fig. ). The findings, along with measurements of 2.2 × 1.8 × 1.9 cm, are consistent with the diagnosis of a Gartner cyst. No changes have been found in the cyst during follow-up to date. Fig. 3 a cystic lesion on the right wall of the vagina near the fornix. b The ultrasound showed a thin wall cyst with anecoic content on the right side wall of the vaginaabCase 4 – follow-up for 2 yearsA 49-year-old mixed-ethnic woman, for 2, was referred to our gynecological clinic due to a nomadic mass within her vagina. The mass had been evident for about 2 years, without symptoms. He had a history of endometrial polyps and uterine fibroids. A pelvic test revealed a cystic lesion of 2 × 2 cm on the right wall of your vagina (Fig. ). The dough was soft and could be manually compressed without difficulty. A pelvic ultrasound confirmed a cystic lesion in this region of your vagina. She was treated conservatively and did not have a cyst growth of interval or change in the cyst characteristics in follow-up. Fig. 4Cystic injury of 2×2 cm in the right wall of the vagina Debate This is one of the few studies of Gartner cysts with a series of consecutive cases followed over a long period of time that were exclusively subject to clinical observation. Most of the case series presented in the literature usually present patients who were surgically treated []. The follow-up of these patients varied from 2 to 17 years. In these four cases the location of cysts was the right wall of the vagina. Gartner cysts are typically small with an average diameter of 2 cm. However, these cysts can increase their size and be confused with other structures, such as cystocele and uterine prolapse []. In fact, in this series, the size ranged from 1.5 to 4.2 cm. In all cases, the diagnosis was performed incidentally during the routine pelvic examination and most injuries were asymptomatic. Only one of the four women had a strict urethra with a recurring UTI history, but this condition had no relation to the presence of the cyst (). Transvaginal ultrasound was the test of choice for diagnostic confirmation (Fig. ). Research of the characteristics of these lesions can be performed with imaging tests of the urinary tract, such as ultrasound and magnetic resonance. Intravenous skinography and computed tomography are additional tests that may be requested []. Treatment depends on the symptoms and desire of the patient. In the cases presented in this study, women were asymptomatic and decided to be clinically observed. In this situation, surgery is not usually done because this type of surgery may be complex and is not recommended unless the patient has severe symptoms []. When a patient is symptomatic, the initial procedure may involve cyst drainage, injection or aspiration, and intra-cystic tetracycline []. In large, symptomatic or recurrent cysts, excision or marsupialization is indicated []. Cytric marsupialization is a simple minimally invasive procedure, which creates minimal surgical scars and results in the pathological diagnosis of a Gartner duct cyst. Long-term follow-up after that procedure has proven its effectiveness without proven side effects or recurrence []. Management strategies for multiloculated recurrences include regular surveillance, sclerotherapy and marsupialization []. In older patients, a mass wall biopsy is recommended to exclude neoplasia; however, the malignant transformation of Gartner cysts is extremely rare []. Conclusions Despite the small number of cases of Gartner cysts, this study shows that conservative treatment can be a safe choice for asymptomatic patients. However, more studies are needed with more women in older age groups to better define the behavior of these patients. ReferencesEilber KS, Raz S. Benign cystic lesions of the vagina: a literature review. J Urol. 2003;170:717–22. Siegelman ES, Outwater EK, Banner MP, Ramchandani P, Anderson TL, Schnall MD. High resolution MR images of the vagina. X-ray. 1997;17:1183–203. Ohya T, Tsunoda S, Arii S, Iwai T. Diagnosis and treatment for the persistent cyst of the Gartner duct in a baby: A case report. J Pediatr Surg. 2002;37:E4. Castagnetti M, Cimador M, De Grazia E. Diagnostic laparoscopy at the Gartner conduit cyst. J Pediatr Urol. 2008;4:173-5. Troiano RN, McCarthy SM. Mollerian duct anomalies: image and clinical problems. Radiology. 2004;233:19–34. Inocencio G, Azevedo S, Braga A, Carinhas MJ. Great Gartner cyst. BMJ Case Rep. 2013. doi:. Marisa RN, Oliva E. Gynecological pathology. Philadelphia: Elsevier Health Sciences; 2009. Molina Escudero R, Navas Martinez MC, OA Castle. Vaginal Gartner cysts: clinical report of four cases and bibliographic review. Arch Esp Urol. 2014;67:181-4. Katz VL. Benign gynecological lesions. In: Integral Gynecology. 6th edition. Philadelphia: Elsevier Mosby; 2012. p. 936. Abd-Rabbo MS, Atta MA. Aspiration and tetracycline sclerotherapy: a novel method for managing vaginal and vulvales cysts. Int J Gynaecol Obstet. 1991;35:235-7. Binsaleh S, Al-Assiri M, Jednak R, El-Sherbiny M. Gartner duct cyst simplified treatment approach. Int Urol Nephrol. 2007;39(2):485-7. Emmons SL, Petty WM. The conduit cysts of the recurring giant Gartner. A two-case report. J Reprod Med. 2001;46(8):773-5. Bats AS, Metzger U, Le Frere-Belda MA, Brisa M, Lecuru F. Malintentional transformation of the Gartner cyst. Gynecol Int J. 2009;19:1655-7. Recognition The authors are grateful to all patients. Contributions from the authors SSR was an important contributor in the writing of the manuscript. The Commission on Human Rights, the Committee of the Red Cross, the Committee of the Red Cross, the Committee on the Rights of the Child and the Ministry of the Red Cross made equal contributions. All authors read and approved the final manuscript. Competing interests The authors declare that they have no competing interests. ConsentThe written informed consent was obtained from the patients for the publication of this case report and any accompanying image. The Editor-in-Chief of this journal can consult a copy of the written consent. Author's information Affiliates Department of Obstetrics and Gynaecology, Faculty of Medicine, University of Brasilia DF, Campus Universitário Darcy Ribeiro, Brasília, DF, 70910-900, BrazilSalete S. Rios, Lara Cristina R. Pereira, Carla B. Santos, Ana Carolina R. Chen, Juliana R. Chen & Maria de Fátima B. Vogt You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in You can also search this author in Correspondence to the correspondent Law and permits Open Access This item is distributed under the terms of the Creative Commons 4.0 International License (S), which allows the use, distribution and reproduction without restrictions in any medium, provided that you give appropriate credit to the original (s) author(s) and source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication () exemption applies to the data available in this article, unless otherwise stated. Open access About this article Cite this articleRios, S.S., Pereira, L.C.R., Santos, C.B. et al. Conservative treatment and follow-up of Gartner vaginal duct cysts: a number of cases. J Med Case Reports 10, 147 (2016). https://doi.org/10.1186/s13256-016-0936-110, Received: 02 December 2015Accepted: 06 May 2016Published: 02 June 2016DOI: KeywordsPublication: Journal of Medical Case Reports ISSN: 1752-1947Contact us By using this website, you agree to our , , and politics. We use at the center of preferences. © 2021 BioMed Central Ltd unless otherwise indicated. Part of .

Gartner's duct cyst - Wikipedia

Gartner's Duct Cyst | NEJM

Figure 3 from Symptomatic Gartner Duct Cyst in A Newborn: Diagnosis and Management | Semantic Scholar
Journal of Nephrology : Journal of Urology | Juniper Publishers

Gartner duct cyst | Radiology Reference Article | Radiopaedia.org
Vaginal cysts Information | Mount Sinai - New York
A Case of Gartner's Cyst of the Vagina - MedCrave online

Gartner duct cyst | Radiology Case | Radiopaedia.org

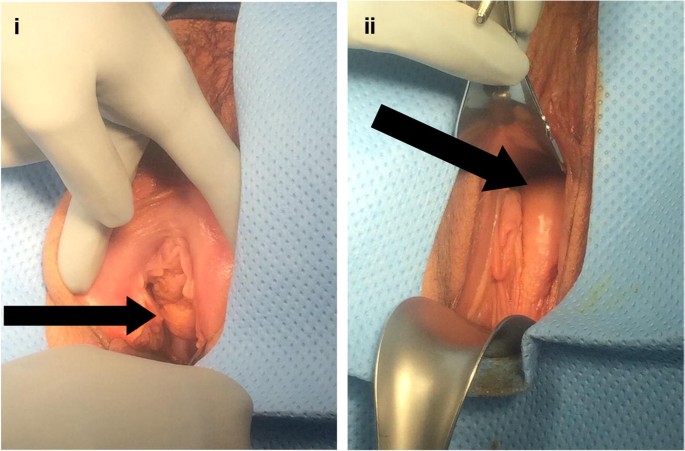
Excision of Vaginal Cysts - Female Pelvic Surgery

A Case of Gartner's Cyst of the Vagina - MedCrave online
Gartner Duct Cyst - Reproductive - Medbullets Step 1

EPOS™

Congenital urogenital anomalies that are associated with the persistence of Gartner's duct: A review - American Journal of Obstetrics & Gynecology
Gartner Duct Cyst: CT and MRI Findings | SpringerLink

Resident and Fellow Education Feature What Is That Cyst? Common Cystic Lesions of the Female Lower Genitourinary Tract | RadioGraphics
130 Gartner Duct Cyst | Radiology Key

Journal of Postgraduate Gynecology & Obstetrics: Half Dumbbell-shaped Gartner's Cyst Presenting As Paraurethral Cyst
A Case of Gartner's Cyst of the Vagina - MedCrave online

Figure 3 from Complex malformations of the urogenital tract in a female dog: Gartner duct cyst, ipsilateral renal agenesis, and ipsilateral hydrometra. | Semantic Scholar

SAG Pelvis (Transabdominal) Gartner's Duct Cyst

PDF) Neonatal Gartner Duct Cyst: Two Case Reports and Literature Review
Benign tumours,cysts
Vaginal cysts Information | Mount Sinai - New York

Gartner Duct Cysts of Vagina
Benign Lesions of the Vaginal Wall | Clinical Gate
Conservative treatment and follow-up of vaginal Gartner's duct cysts: a case series | Journal of Medical Case Reports | Full Text

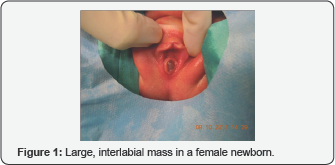
Diagnosis and treatment for persistent Gartner duct cyst in an infant: A case report - Journal of Pediatric Surgery
Symptomatic Gartner Duct Cyst in A Newborn: Diagnosis and Management
Gartner duct cyst | Radiology Reference Article | Radiopaedia.org
Benign tumours,cysts

Infected gartner duct cyst | Eurorad

Pin on OB/Gyn Ultrasound 101 Mod 2

A schematic image of the Gartner's duct cyst observed in the present case. | Download Scientific Diagram

EPOS™
barber layout 37465

Excision of Vaginal Cysts | Obgyn Key

Gynaecology | 3.3 Vagina : Case 3.3.2 Miscellaneous vagina and external genitalia | Ultrasound Cases

Gartner duct cyst | Radiology Reference Article | Radiopaedia.org | Cysts, Radiology, Duct

Ultimate Radiology : Gartner Duct Cyst (Vaginal Cysts)
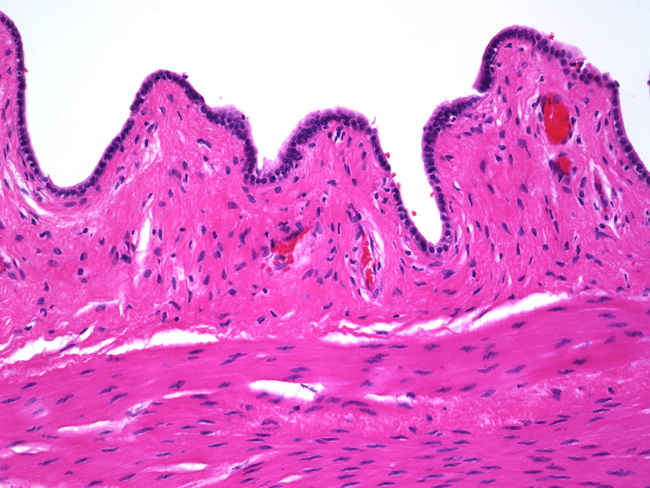
Webpathology.com: A Collection of Surgical Pathology Images
Posting Komentar untuk "gartner’s duct cysts"